Urological Cancers
Prostate cancer
Prostate cancer is the most common cancer in males in Scotland, with approximately 3,100 new cases diagnosed every year. Risk increases with age and approximately 99% of cases are diagnosed in men aged over 50 years. Risk of prostate cancer is increased if a first degree relative has had prostate cancer or if there is a family history of BRCA associated breast or ovarian cancer. The presence of a BRCA mutation increases risk substantially, in particular for early or aggressive disease in BRCA2 mutation. In the UK, the lifetime risk of prostate cancer in black men (1 in 4) is double that of all men combined (1 in 8).
Men presenting with unexplained possible symptoms and signs suggestive of prostate cancer such as changes to urinary patterns, erectile dysfunction, unexplained visible haematuria, lower back pain, bone pain or weight loss should have a digital rectal examination and a prostate specific antigen (PSA) test with counselling. A PSA test may be raised within three days of ejaculation or six weeks of a proven UTI, catheterisation or other invasive procedure, such as prostate biopsy. 5 alpha reductase inhibitors such as finasteride may reduce the PSA level. It should be noted that the majority of men with prostate cancer have no symptoms at all.
Bladder and kidney cancer
Visible haematuria is the most common presenting symptom for both bladder and kidney cancer. Other presenting features include loin pain, renal masses, non-visible haematuria, anaemia, weight loss and pyrexia. Both cancers are uncommon, with around 800 new bladder and 950 new kidney cancers each year. There is evidence of an association between bladder cancer and a raised white cell count on a blood test in people aged over 60.
Testicular and penile cancer
Although scrotal swellings are a common presentation in primary care, testicular cancer is relatively rare, with around 200 new cases per annum, of which approximately 72% are in men between 15 and 45 years. Solid swellings affecting the body of the testis have a high probability (> 50%) of being due to cancer. Because of the potential for rapid progression of testicular cancers, specialist services should consider triaging referrals in order to expedite such cases. Cancer of the penis is rare, with around 60 new cases each year in Scotland, but its incidence is rising. Sexually transmitted disease should be excluded and referred only if a lesion persists after treatment.
All people presenting with symptoms or signs suggestive of urological cancer should be referred to a team specialising in the management of urological cancer, depending on local arrangements.
Urgent suspicion of cancer referral
Prostate Cancer
- Evidence from digital rectal examination of a hard, irregular prostate
- Elevated or rising age-specific Prostate Specific Antigen (PSA). Rough guide to normal PSA levels (ng/ml):
- Less than 60 years < 3
- Aged 60–69 years < 4
- Aged 70 years and over < 5
These figures are a pragmatic aid based on clinical consensus. The principles of Realistic Medicine should be applied when considering referral and, in older men, routine or no referral may be appropriate for PSA levels of:
- Aged 80-85 years > 10
- Aged 86 years and over > 20
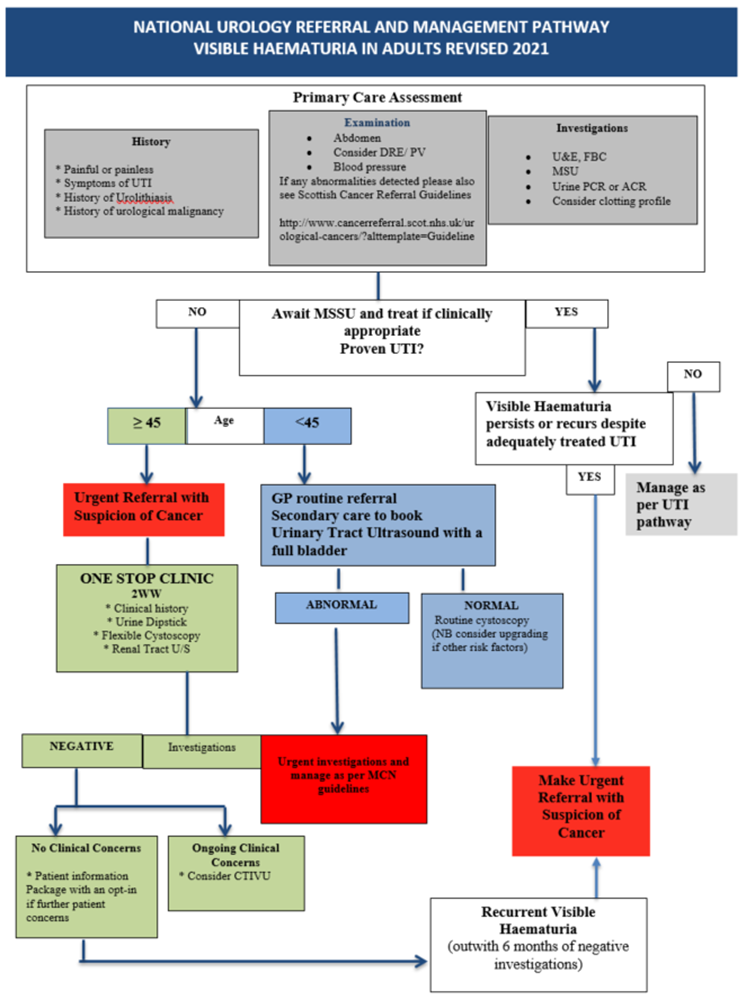
Bladder and kidney cancer
- Aged 45 and over and have unexplained visible haematuria without urinary tract infection
- Visible haematuria that persists or recurs after successful treatment of urinary tract infection
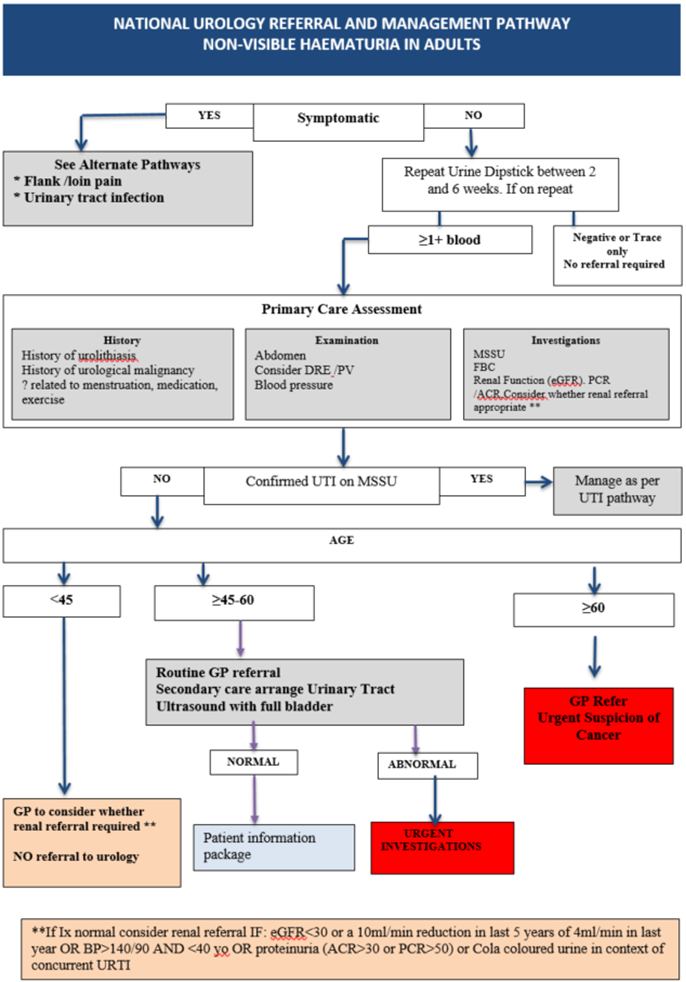
- Age 60 and over and have persistent unexplained non-visible haematuria in the absence of urinary infection
- Abdominal mass identified clinically or on imaging that is thought to arise from the urinary tract
(see flowcharts below)
Testicular and penile cancer
- Non painful enlargement or change in shape or texture of the body of the testis
- Suspicious scrotal mass found on imaging
- Men considered to have epididymo-orchitis or orchitis which is not responding to treatment
- Any non-healing lesion on the penis or painful phimosis
Routine referral
- Elevated age-specific PSA where urgent referral will not affect outcome due to age or comorbidity
- Asymptomatic persistent non-visible haematuria without obvious cause (age 45-60)
- Unexplained visible haematuria < 45 years of age
- Patients over 40 who present with recurrent UTI associated with any haematuria